- Shanghai, China
- [email protected]
- +86-21-58189111
Intervertebral discoscope is a medical device that uses endoscopic technology to remove the nucleus pulposus tissue of intervertebral disc herniation with surgical instruments.
Introduction to Discoscopy
Lumbar disc herniation (LDH) is a common disease that causes chronic low back and leg pain. The main cause of the disease is based on the degeneration of the intervertebral disc, especially when the degeneration of the annulus fibrosus is larger than the degeneration of the nucleus pulposus that it contains. Accelerated, prone to disc bulge or herniation. Most patients can achieve better clinical results through conservative treatment, and surgical treatment can be considered for those with poor results from strict conservative treatment; traditional open surgery has large trauma, heavy bleeding, severe postoperative pain, and extensive damage to the muscles and soft tissues of the lower back during the operation. Peeling causes damage. Studies have shown that this soft tissue injury is one of the main causes of chronic low back pain in patients after surgery.
In 1963, Smith injected chymopapain into the intervertebral disc of patients, which started a new era of minimally invasive treatment of lumbar intervertebral disc disease. In 1997, Smith and Foley took the lead in applying microendoscopy technology to LDH surgery. Minimally invasive treatment of LDH is now It has become the most active field of minimally invasive spine surgery and is more and more widely used in clinical practice. The main minimally invasive techniques include percutaneous discectomy, chemical nuclear fusion, nucleoplasty, and microscopy and endoscopy-assisted techniques. Minimally invasive technology has the advantages of less trauma, definite curative effect, fewer complications, no damage to spinal stability, less pain for patients, and faster recovery in the treatment of LDH.
However, while advocating minimally invasive surgery, traditional open surgery cannot be completely denied. Traditional posterior open surgery still occupies the mainstream position and often becomes the remedy for minimally invasive surgery. The two are not mutually exclusive, and each has its own strengths, and different treatment methods should be selected according to different situations. It is necessary to strictly grasp the principles, indications and contraindications of various therapies, and to adopt individualized treatment plans for patients, so that these technologies can be continuously improved and innovated, so as to be truly minimally invasive.
advantage
1. Wide range of indications, can treat lumbar disc herniation and lumbar spinal stenosis;
2. Small wound (about 1.5cm), less tissue damage, less bleeding, and short operation time;
3. High safety performance, magnifying 60 times under the microscope, can clearly distinguish the tissue under the microscope, and avoid nerve root damage;
4. The postoperative bed rest time is short and the recovery is fast, and outpatient surgery can be performed;
5. The cost of comprehensive treatment is reduced;
6. High degree of patient acceptance;
7. High-definition vision, easy to deal with lesions that are easy to ignore;
8. The whole operation process is recorded, which is convenient for case discussion and academic exchange.
Common classification
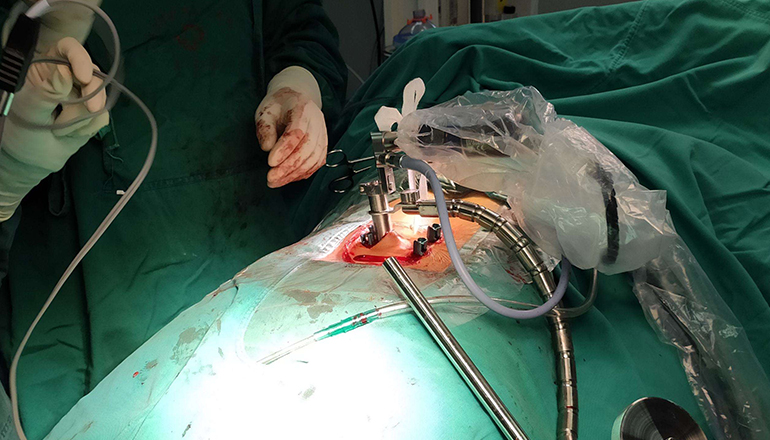
Intervertebral discoscopy (MED) is to insert a working cannula into the intervertebral disc, and enter the channel containing the illumination and image transmission system to the site of the disc herniation. A surgical technique for removing protruding nucleus pulposus tissue, avoiding the nerve root. According to the different approaches, intervertebral discoscopy can be divided into two categories.
1. Discoscopy with posterolateral approach or transforaminal approach
This approach allows access to the epidural space through the intervertebral foramen, and the "triangular workspace" facilitates correct positioning during surgery. This type of intervertebral discoscope is especially suitable for distal-lateral intervertebral disc herniation and nucleus pulposus herniation in the intervertebral foramen, and can also be used for paracentral intervertebral disc herniation. This approach does not require bone manipulation, so it is less disruptive to spinal stability and saves operative time. Although this approach also enters the epidural space, local scarring is rare. Some special instruments, such as automatic suction punch, planer, and 90° bendable laser probe for pyknosis and electrocoagulation for hemostasis, have expanded the indications of this technology. Even foraminal stenosis, which was originally considered a contraindication, is now listed as an indication for surgery. However, the general spine surgeon is not familiar with this approach, so the use of this technique requires special training over a period of time.
2. Intervertebral discoscopy through the laminar approach
This approach adopts the traditional surgical approach, which is familiar to the majority of spine surgeons. Therefore, it has certain advantages in learning to operate and use, and it has less muscle damage. Due to the need to deal with the lamina bone and ligamentum flavum, the operation time is increased. This type of intervertebral discoscopy is relatively difficult for the treatment of distal lateral or foraminal herniation, but it is quite convenient for central intervertebral disc herniation or free nucleus pulposus into the spinal canal, and can perform lateral recess enlargement and vertebral body enlargement. Resection of posterior edge osteophytes.
After several stages of development and innovation, the movable intervertebral discoscope has been used in clinical practice. Its advantages are: movable type: not fixed with the operating bed; self-balancing type: it can balance and stand upright in the incision. The surgical instrument moves and swings; the endoscope and the work are usually at a 12° angle, and the field of view is not dead; It solves the shortcomings of the previous limited field of view and small operation space; the operation direction of the instrument is limited, and it cannot be tilted or swung at will; and all the instruments pass through the same channel and interfere with each other.
Leave a Comments